case 46 : A 65 yr old male with Delirium under evaluation
Saturday, 21 November 2020
A 65 yr old male with Delirium under evaluation , Pre-renal AKI, Non healing ulcer over right foot, Anemia: microcytic hypochromic under evaluation
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
CASE PRESENTATION
A 65year old male patient shepherd by occupation came with c/o ulcer over dorsum of lt foot since 6 months and disoriented speech since 1 day.
Pt was apparently asymptomatic 6months ago then he sustained trauma to his right lower limb and developed ulcer and right lower limb edema. Pt has been on regular dressings for the ulcer with RMP.
3months ago pt developed left lower limb edema also
1week ago h/o giddiness and fall(pt did not eat food that day),pt did not remember the event of fall but according to attendors there was no loss of consciousness,no trauma,no seizures
Since 5days c/o involuntary micturation,involuntary passing stools and spitting everywhere,altered behaviour, irrelevant talk,visual hallucinations,no orientation to person place
Pt not sleeping since 4days
Decreased appetite since 1week
Occasional alcoholic
smoker since 40 years
Past history:
Not a k/c/o DM,HTN,CAD,CVA, Epilepsy
Personal history:
Mixed diet
Decreased appetite
Sleep not adequate
Bowel and bladder involuntary
Occasional alcoholic
Smoker since 40 yrs
O/E
Pt is conscious, not orientated to time,place and person, thin built
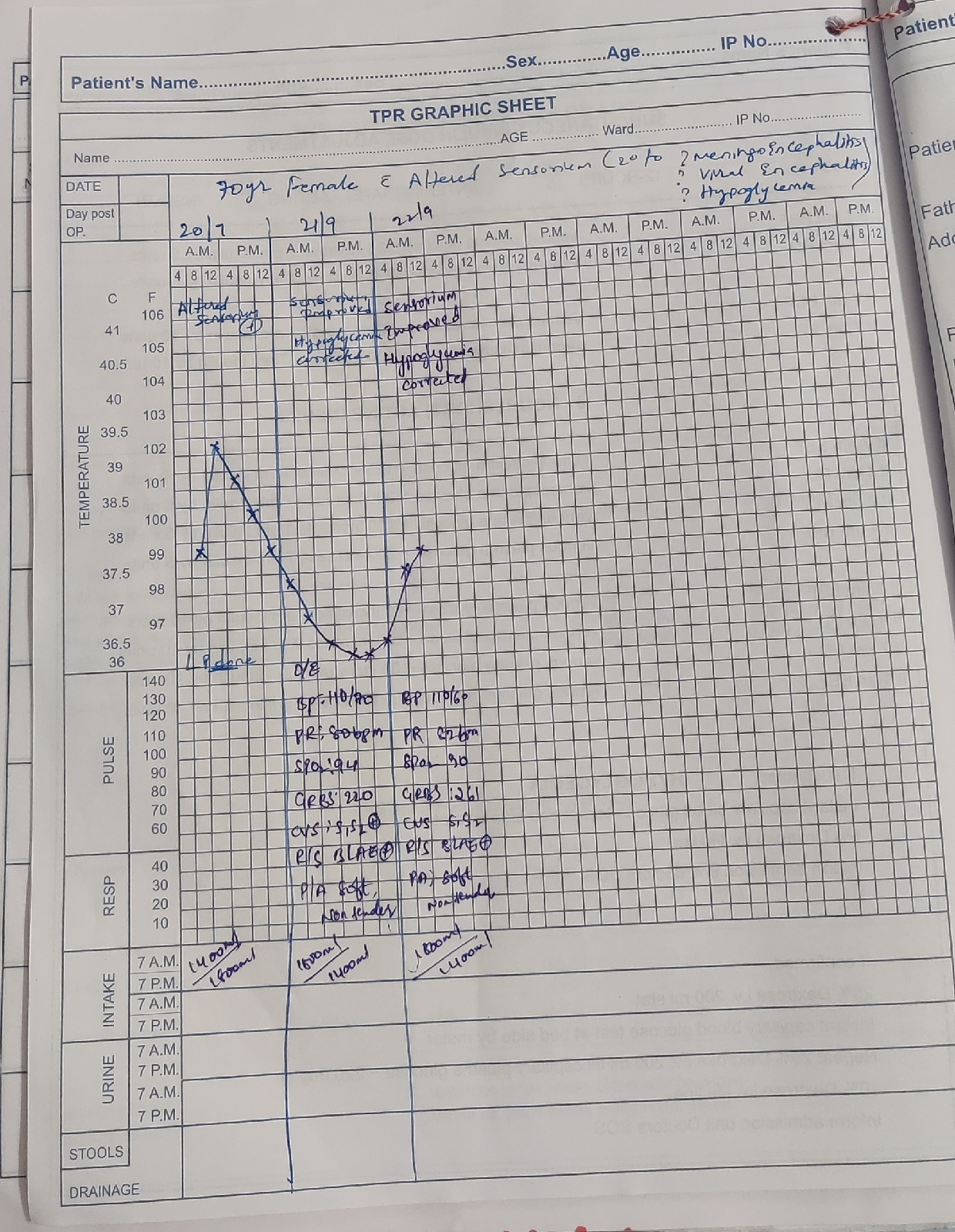
Vitals
Pt is Afebrile
BP - 110/70 mmhg
PR - 82bpm
RR - 16 CPM
CVS - S1S2 heard
RS - BAE present
P/A - soft , non tender
CNS - No neck rigidity, signs of meningitis
Motor and sensory not elicitable
Psychiatry notes:
Day 1:
C/O : sleep disturbance, irrelevant talk , irritability, self talking, decreased appetite since 3 days
Pt was apparently asymptomatic 1week back,he was sitting in the field during day time, pt fell down and was brought to home by village people, pt was taken to a nearby hospital, after 3 days pt started behaving abnormally ,sleep decreased, appetite decreased,self talking,visual hallucinations, irrelevant talk, spitting frequently, involuntarily passing urine
H/O consumption of whiskey 90ml , toddy 500ml occasionally, h/o tobacco smoking since 20 yrs , 2 cigarettes per day , stopped 3 months back (OD denies withdrawal symptoms)
No H/O suspiciouness ,self smiling, low mood , crying spells, fear , palpitations , repititive thoughts, suicidal ideation
MSE - GAB- pt is sitting on bed , frequently trying to go outside of ward
ETEC negative
PMA Normal, rapport CNBE
further MSE CNBE
No Orientation to time ,place , person
DAY 2:
Pt reports to have slept well, decreased irritability
MSE - GAB : pt sitting on the wheel chair, responding to oral commands. PMA normal ETEC present not sustained, rapport established with difficulty
RT increased, relevant, coherent
Affect - dysphoric
Thought and perception - CNBE
Not oriented to time , orientated to place, person.
INVESTIGATIONS:
LFT
TB 0.66
DB 0.2
SGOT 17
SGPT 17
ALP 279
TP 4.7
Alb 2
RBS 70
DIAGNOSIS:
Delirium under evaluation
Pre-renal AKI
Non healing ulcer over right foot
Anemia:microcytic hypochromic under evaluation
TREATMENT:
1. RF FEEDS 200 ML MILK WITH PROTEIN POWDER 2ND HRLY, 100ML PLAIN WATER4TH HRLY
2. IVF 1 UNIT NS , 1 UNIT DNS @ 75ML/HR
3. INJ OPTINEURON 1AMP IN 100ML NS/IV/OD
4. INJ PANTOP 40MG IV/OD
5. TAB OROFER XT PO/BD
6. TAB OLANZAPINE 2.5 MG PO/BD
7. INJ HALOPERIDOL 2.5 MG IM
8. INJ LORAZEPAM 2 MG IM/ SOS IF SLEEPLESS
9. ZYTEE GEL FOR L/A
10. GRBS CHARTING 6TH HRLY
11. I/O CHARTING
12. SYP LACTULOSE 15 ML PO/BD


















Comments
Post a Comment