Case 41 - ALTERED SENSORIUM SECONDARY TO RECURRENT HYPOGLYCEMIA (RESOLVED) WITH VIRAL MENINGO ENCEPHALITIS (RESOLVED) WITH K/C/O DM-2 WITH CHOLILITHIASIS WITH LEFT CORTICAL CYST
A 70yr old female with involuntary movements in upper and lower limb
MEDICINE E LOG BOOK
“This is an online e log book to discuss our patient’s de- identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patient’s clinical problems with collective current best evidence based inputs. This e-log book reflects my patient centered online portfolio and your valuable inputs on the comments is welcome.”
CHIEF COMPLAINT
Patient came to casualtiy with altered sensorium with involuntary movement in Right upper limb since 12:00 am, c/o loss of speech and no movement in left upper limb and lower limb after 12:00 am pt had h/o 3 episodes of involuntary micturition since 5 days , c/o one episode of fever 2 days back which was relieved on medication . On the way to the hospital PT grbs was found to be 15 mg/dl and a 25 d was connected after which the grbs was 131 mg /dl
HISTORY OF PRESENTING ILLNESS
Pt was apparently asymptomatic 2days ago then she developed b/l involuntary movements in upper and lower limb, loss of speech and recognition of people. Associated with drooling of frothy saliva from mouth,up rolling of eyes, biting of tongue. No h/o fever,nausea, vomiting, headache, blurring of vision, diarrhoea, constipation
PAST HISTORY
K/c/o DM since 2 yrs and on medication metformin 500 mg and pt medication was changed by local practioner to glimi m 1 8 days back from the presentation to the casualtiy.
Not a k/c/o epilepsy, asthma, HTN, tuberculosis
No H/o previous surgeries
PERSONAL HISTORY
Diet: mixed
appetite: normal.
sleep: adequate,
b&b movt: regular
addiction: tobacco chewing
FAMILY HISTORY no significant family hisory
General examination
Pt is drowsy
No pallor, icterus, cyanosis, clubbing generalized lymphadenopathy and oedema.
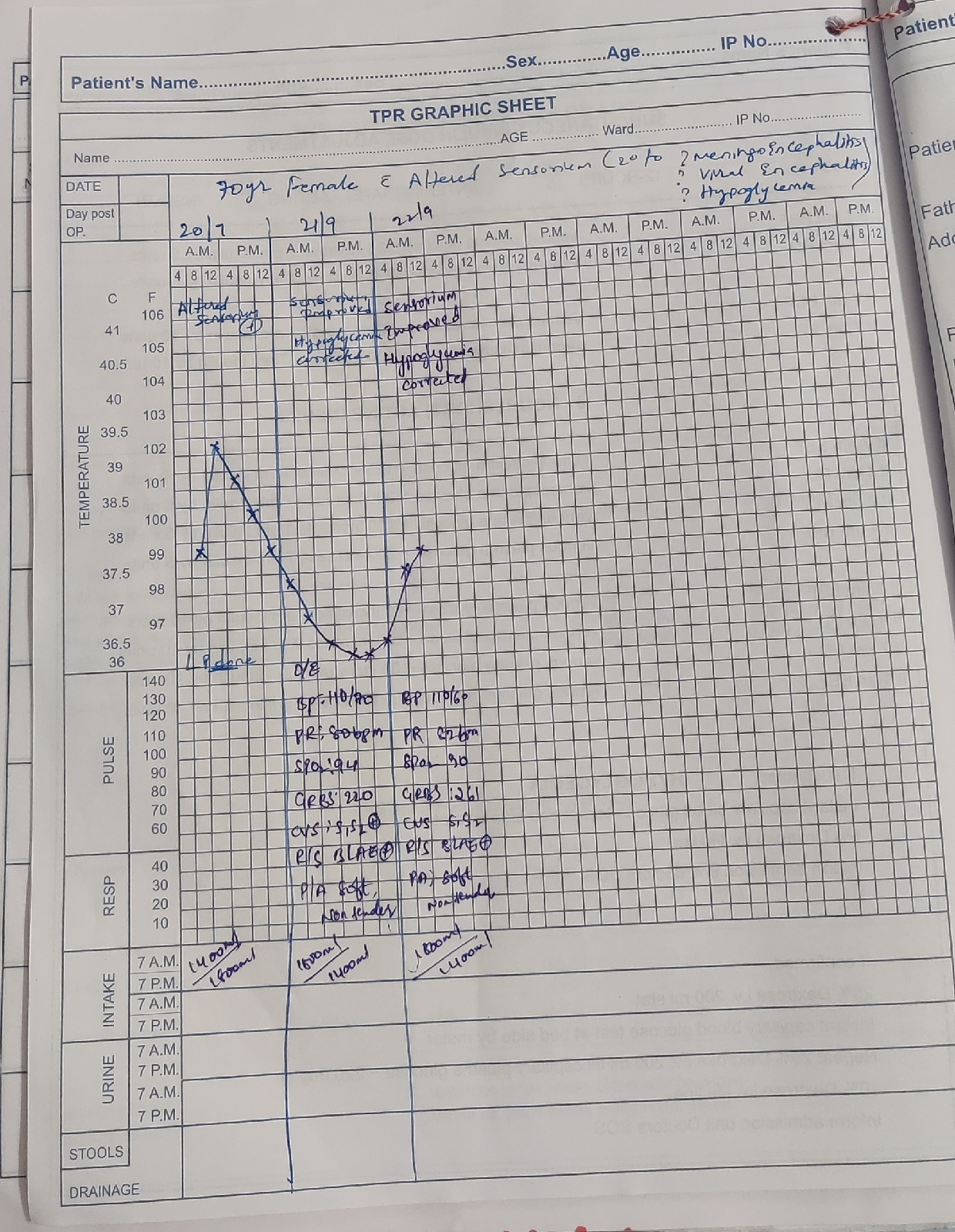
Vitals
Bp 150/100 mmhg
Pulse 97 bpm
RR 20 cpm
Temperature 98.6
Spo2 97
Grbs 81 mg/dl
SYSTEMIC EXAMINATION
CNS
Upper limb lower limb
Rt left Rt left
Tone normal normal increased increased
Power 3/5 3/5 3/5 3/5
Reflexes right left
Biceps ++ ++
Triceps ++ ++
Supinator ++ ++
Knee ++ ++
Ankle
Plantar flexon mild extension
https://youtube.com/shorts/-7N-84kWxAI?feature=share.
CVS S1,S2 +,no added murmurs
R/S NVBS heard
P/A soft and non tender
Provisional diagnosis:
ALTERED SENSORIUM SECONDARY TO RECURRENT HYPOGLYCEMIA (RESOLVED) WITH VIRAL MENINGO ENCEPHALITIS (RESOLVED) WITH K/C/O DM-2 WITH CHOLILITHIASIS WITH LEFT CORTICAL CYST



Comments
Post a Comment