14/M, massive splenomegaly
This is an online Elog book to discuss our patient deidentified health data shared after taking his/ her guardians sign informed consent
Here we discuss our individual patient problems through series of inputs from available Global online community of experts with n aim to solve those patient clinical problem with collect current best evidence based input
This Elog also reflects my patient centered online learning portfolio.
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competancy in reading and comprehending clinical data including history, clinical finding, investigations and come up with a diagnosis and treatment plan
CONSENT AND DEIDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed through out the piece of work whomsoever .
Case history :
14 yr old male came to the opd with complaints of pain abdomen in the left side of the abdomen since the past 15-20 days along with cold and cough since the past 10 days.
He was having pain abdomen and noticed a swelling in the left side of the abdomen since the past 15-20 days along with cold and cough associated with scanty sputumA for the past 10 days. On asking him to elaborate about pain abdomen, it was of dragging type, non radiating, no associated symptoms and was started on symptomatic management.
General examination showed thin built moderately nourished with pallor with cervical and inguinal lymphadenopathy and massive splenomegaly
lungs clear and Apex beat localised to 5th intercostal space with left parasternal pulsations.
no focal deficits in neurological examination.
General examination:
Initial investigations revealed
HEMOGRAM :
HAEMOGLOBIN #7.8
TOTAL COUNT # 1.600
NEUTROPHILS #31
LYMPHOCYTES #42
EOSINOPHILS # 09
MONOCYTES#18
BASOPHILS 100
PCV #24.8
MCV #76.5
MCH # 24.0
MCHC # 314
RDW-CV # 19 3
RDWV-SD 53 9
RBC COUNT # 3.25
PLATELET COUNT 20,000
SMEAR
Microcytic Hypochromic with few normocytes and pencil forms seen
WBC counts reduced on smear with monocytosis
PLATELETS counts reduced on smear
No hemoparasites seen
IMPRESSION
pan cytopenia
LIVER PROFILE :
Total Bilurubin 0.79
Direct Bilurubin 0.18
SGOT(AST) 10
SGPT(ALT) 15
ALKALINE PHOSPHATE 163
TOTAL PROTEINS #4.5
ALBUMIN # 2.6
A/GRATIO 1.43
COAGULATION PROFILE :
PT 17 sec
APTT 33 sec
INR 1.2
RENAL FUNCTION :
Blood urea 10
Serum creatinine 0.5
Sodium 134
Potassium 3.4
Chloride 104
ionised calcium 0.93
LDH 120
Reticulocyte count 0.5
Direct Coombs test positive.
Chest x ray PA view :
USG Abdomen showing portal vein dilatation of 16mm and massive splenimegaly with no ascites.
USG neck showing
1.Diffuse thyroiditis with thyroid nodule in left lobe
2.Bilateral submandibular gland, sialo adenitis secondary to inflammatory changes
3.mild parotiditis with enlarged parotid lymph nodes.
Echo of portal vein : https://youtube.com/shorts/39HT-lJJ6hM?feature=share
2D Echo : https://youtu.be/7NAXqdO4ZDI
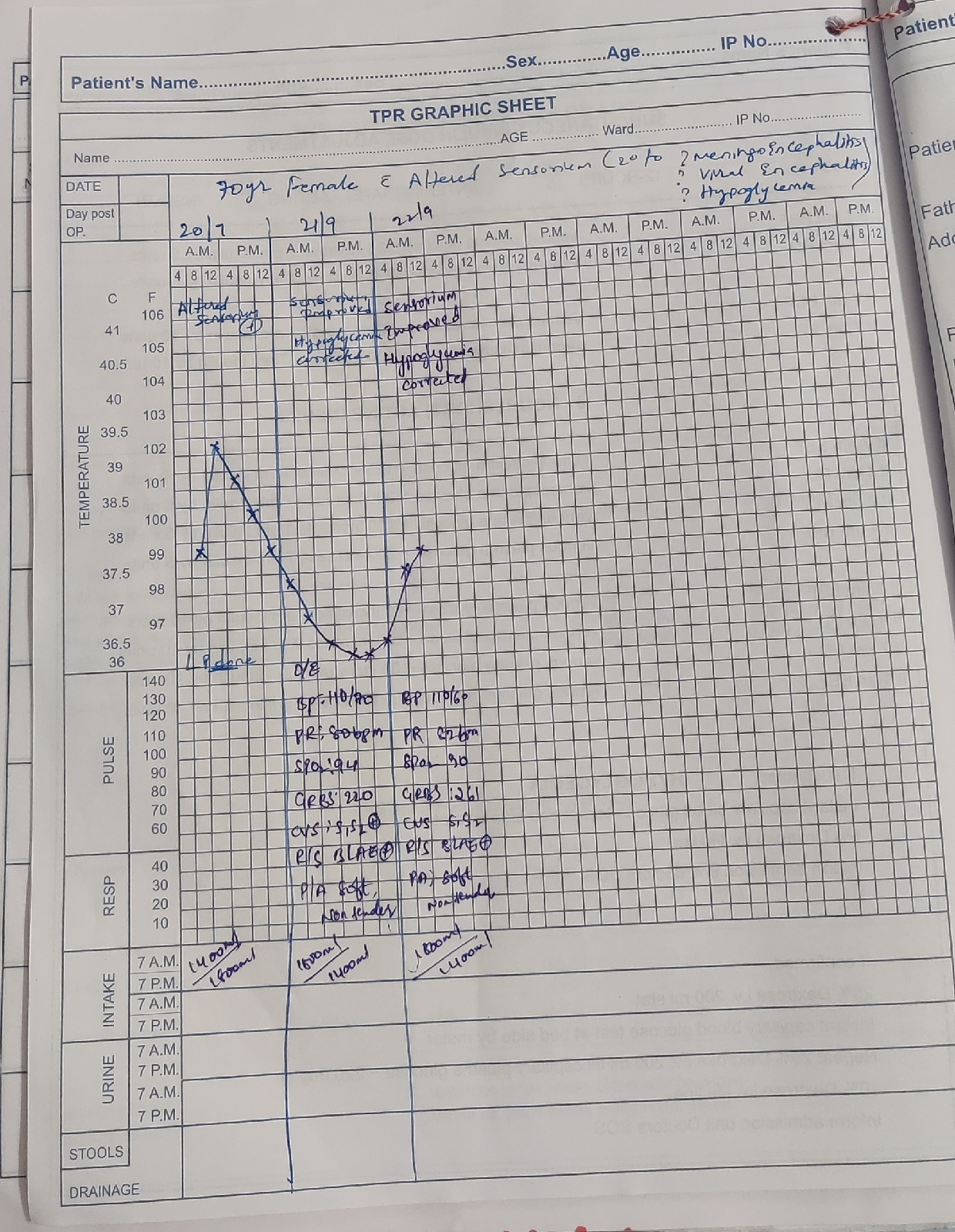
FEVER CHART :

Family history :
He is a 4th order child ,born out of grade 4 consanguinous marriage, He has 2 elder brothers and one elder sister - who expired at 5 years of age, His sister was the first child and she was assymoptomatic till 2 years of age ,then she had shortness of breath and was rushed to hospital,where here condition detiorated and got admitted .They were told that she had splenomegaly and Her blood counts were decreasing .She was given multiple blood transfusions every 25 days for one year inspite of that she remained anemic ,she also underwent bone marrow biopsy twic, was advised splenectomy, but they denied. According to parents she was given steriods also for one year before death .she never had jaundice or recurrent infections.
Elder brother is 19 year old and second brother is -16 years old . Second one had history of fever ,white coloured loose stools at the age of 5 years ,for which they went to near by hospital .He was given some medications and it got resolved .But he was said to have anemia ,and he recovered according to parents with some medications.There was no jaundice and no history of blood transfusion.
Pedigree chart :
Patient's birth history :
He is the youngest of all. He was born out of normal vaginal delivery with 4.25kgs birth weight, cried immediately after birth. He had jaundice at birth ,that resolved spontaneously .? Physiological jaundice. He is Immunised as per schedule .
Antenatal history:
Mother had regular AN checkups , had 2 doses of T.T, Had IFA psophylaxis, No history of
DM/HTN/TB, No history of prom/APH, Birth history : SPVD cried immediately after birth, birth weight 4.25Kgs, Post nenotal history : MSL - NICU admission for 1 day, excesive Breast feeds from 2nd day of life, exclusive breast feeds till 6 months, F/B weaning started with cerelac continued till 10 months, than child had loose motions/, stopped cerelac / Breast feeding.
INITIAL PROBLEM
Around 12months of his age, he was brought with complaints of Not gaining weight since last 3 months with delayed mile stones since last 3 months, loose motions/ vomitings on & off since 3 months.
He was apparently normal 3 months back than child was not gaining weight, loose
motions greenish in colour, watery in character 25 - 30 times a day, not associated with blood & mucus, vomitings 4 - 5 times, non bilious/ non projectule, No history of ear dishcarge, History of recurrent cough and cold with no history of decrease in urine out put, No history of cyanosis.
During the hospital stay he was admitted in ward started IV fluids and blood investigations were sent blood investigation were s/o severe Hypokalaemia as low as 1.5 with leucocytosis, Child potassium was corrected over 24 - 26hours, child stool examination showed bacteria ( E. coli ) and child started on IV antibiotics along with IV anti fungal, Child responded well and general condition improved day by day, Child given 2 units of FFP and child started on oral diet, avoiding wheat diet, child shown to another Paediatrician Suspected as celiac disease, Child blood sent for Anti endomysial antibodies, ( no availability of report ) his general condition improved and stool consistency changed to semisolid, child parents were counselled about the oral diet and was discharged
On further asking parents, they told he used to have recurrent colds ,cough and fever. He used inhalers for 1 year during winters in childhood though he wasn't admitted at any point, and there was no history of pneumonia.
Childhood history :
At 9 years of age August, 2016 - parents noticed neck swelling and he had difficulty in swallowing they took him to ENT doctor ,later referred to endocrinologist ,where he was diagnosed with hyperthyroidism, USG showed diffuse enlargement of both lobes of thyroid gland with altered echotexture ?Goitre with bilateral jugular lymphadenopathy. FNAC was done showing features suggestive of hyper plastic goitre. Initial TSH - 0.57, T3,T4 was 217 and 1.8 respectively, he was started with propylthiouracil 50 mg and was asked to review back as of October 2016, TSH was >150 and T3 - 12, T4 was <0.3 and was started intitially on thyroxine supplementation of 25mcg later on increasing to 150,180 and 200mcg over 6 months.
At 12 years of age patient had chicken pox ,resolved over 10 days.
Around late part of December 2021
He gave history of yellowish discoloration of eyes, One episode of bilious vomiting. yellow coloured urine, He was treated by a pediatrician (family doctor) for jaundice ,but as the bilirubin was on increasing trend he was referred to our hospital in the first week of January with the history of above said complaints of 7-10 days
No pale colored stools .
No fever ,pain abdomen ,loose stools.
No cold, cough .
No history of small joint pains .
At that time of presentation :
On examination -
He was thin built .
Height -156 cm
Weight - 32kgs
Jaundice + ,pallor +
Per abdomen -soft, non tender with moderate splenomegaly
Outside investigations -
There is significant drop in hemoglobin from 8.9 to recent HB -5,leucopenia , thrombocytopenia.
With raised bilirubin - both direct and indirect, normal enzymes .
Urine for bile salts and bile pigments + ve
HB electrophoresis - normal .
Serology for HiV ,HBSag , Hcv was negative
Dengue , Malaria ,widal was negative
Hemogram showed -
Normocytic normochromic anemia with HB 5.1
WBC count -1700 ,neutrophils -39% ANC-663 ,Esoniphils -8% .
Platelet count -1.5 lakh
With few microcytes ,tear drop cells ,pencil forms.
Liver profile showing total bilirubin of 6.49, direct amounting to 0.52, with AST,ALT,ALP normal, total proteins of 5.5 and albumin of 3.8
Direct Coombs was positive
USG abdomen showing moderate splenomegaly.
Assessment :
? Spectrum of Autoimmune diseases -
Thyroditis ,? AIHA
Chronic itching of both hands and limbs
? CVID
He was started on methylprednisalone 32mg IV for 5 days later on converted to oral dosage of 30mg and was tapered over 2 months.
And vitamin B12 1000mcg injections through the course of hospital and was continued for 6 months (standard b12 regimen ). And other symptomatic medications.
DAILY SOAP NOTES :
AMC bed 3 14yr old male
Admitted on 26/08/22
DAY 1
HEMOGRAM
Haemoglobin #7.8
Total counts #1600
N#31
L #42
E # 09
M#18
B 00
PCV #24.8
MCV #76.5
MCH # 24.0
MCHC # 31.4
Rbc's #3.25
Platelet count 20,000
THYROID PROFILE :
T3 0.63
T4 13.18
TSH 2.05
S: cough and cold decreased.
O: pt is conscious, coherent,cooperative.
BP: 110/70mmhg
PR: 84/m
RR: 22
Temp: 99.2f
GRBS: 87mg/dl -8am
Spo2: 98%
RS: BAE+ clear
CVS: s1,s2 no added sounds
P/A: not tender, splenomegaly +
CNS:NAD
A: pancytopenia with massive splenomegaly
Thyroditis ,? AIHA, URTI
P: plan of treatment
1.Inj. Neomol 1gm IV SOS
2.Tab dolo 650 mg PO SOS
3.Tab. Levocetrizine 5mg PO SOS
4.Syrup ascoril 10 ml PO BD
5.tab. thyronorm 200mcg, PO OD
6.inj. optineruron 1 amp
7. BP temp charting 6th hourly
DAY 2
HEMOGRAM :
Haemoglobin #8.5
Total counts #2400
N#30
L #50
E # 10
M#10
B 00
PCV #27.3
MCV #76.2
MCH # 23.7
MCHC # 31.1
Rbc's #3.58
Platelet count 40,000
S: cough and cold decreased.
O: pt is conscious, coherent,cooperative.
BP: 110/80mmhg
PR: 89
RR: 24
Temp: 99.2f
GRBS: 83mg/dl -8am
Spo2: 98%
RS: BAE+ clear
CVS: s1,s2 no added sounds
P/A: not tender
CNS:NAD
A: pancytopenia with massive splenomegaly
Thyroditis ,? AIHA, URTI
P: plan of treatment
1.Inj. Neomol 1gm IV SOS
2.Tab dolo 650 mg PO SOS
3.Tab. Levocetrizine 5mg PO SOS
4.Syrup ascoril 10 ml PO BD
5.tab. thyronorm 200mcg, PO OD
6.inj. optineruron 1 amp
7. BP temp charting 6th hourly
AMC bed 3 14yr old male
Admit on 26/08/22
DAY 3
Haemoglobin - 8.7
TLC - 980
Neutrophil’s - 27
Lymphocytes - 60
Eosinophil’s - 03
Monocytes - 10
Platelets - 23,000
S: cough and cold decreased.
O: pt is conscious, coherent,cooperative.
BP: 110/70mmhg
PR: 84
RR: 22
Temp: 99.2f
Spo2: 98%
RS: BAE+ clear
CVS: s1,s2 no added sounds
P/A: not tender
CNS:NAD
A: pancytopenia with massive splenomegaly
Thyroditis ,? AIHA, URTI
P: plan of treatment
1.Inj. Neomol 1gm IV SOS
2.Tab dolo 650 mg PO SOS
3.Tab. Levocetrizine 5mg PO SOS
4.Syrup ascoril 10 ml PO BD
5.tab. thyronorm 200mcg, PO OD
6.inj. optineruron 1 amp
7. BP temp charting 6th hourly.
DAY 4
Haemoglobin - 9.5
TLC - 2400
Neutrophil’s - 39
Lymphocytes - 46
Eosinophil’s - 09
Monocytes - 08
Platelets - 54,000
S: cough and cold decreased.
O: pt is conscious, coherent,cooperative.
BP: 110/80mmhg
PR: 82
RR: 22
Temp: 97.9f
Spo2: 98%
RS: BAE+ clear
CVS: s1,s2 no added sounds
P/A: not tender
CNS:NAD
A: pancytopenia with massive splenomegaly
Thyroditis ,? AIHA, URTI
P: plan of treatment
1.Inj. Neomol 1gm IV SOS
2.Tab dolo 650 mg PO SOS
3.Tab. Levocetrizine 5mg PO SOS
4.Syrup ascoril 10 ml PO BD
5.tab. thyronorm 200mcg, PO OD
6.inj. optineruron 1 amp
7. BP temp charting 6th hourly
DAY 5
Haemoglobin - 9.7
TLC - 4000
Neutrophil’s - 49
Lymphocytes - 36
Eosinophil’s - 05
Monocytes - 10
Platelets - 84,000
S: cough and cold decreased.
O: pt is conscious, coherent,cooperative.
BP: 110/80mmhg
PR: 80
RR: 20
Temp: 97.9f
Spo2: 98%
RS: BAE+ clear
CVS: s1,s2 no added sounds
P/A: not tender
CNS:NAD
A: pancytopenia with massive splenomegaly
Thyroditis ,? AIHA, URTI
P: plan of treatment
1.Inj. Neomol 1gm IV SOS
2.Tab dolo 650 mg PO SOS
3.Tab. Levocetrizine 5mg PO SOS
4.Syrup ascoril 10 ml PO BD
5.tab. thyronorm 200mcg, PO OD
6.inj. optineruron 1 amp
7. BP temp charting 6th hourly
Day 6
Hb - 9.5
TLC - 3000
Plt - 1L
S: cough, cold decreased and left shoulder pain since yesterday
Pain abdomen +
O: pt is conscious, coherent,cooperative.
BP: 110/70mmhg
PR: 90
RR: 18
Temp: 98.2f
Spo2: 98%
RS: BAE+ , adventitious sounds heard at rt and left inframammary region
CVS: s1,s2 no added sounds
P/A: not tender
CNS:NAD
Grbs at 8am: 98mg/dl
A: pancytopenia with massive splenomegaly
Thyroditis
,? AIHA, URTI
P: plan of treatment
.Inj. Neomol 1gm IV SOS
2.Tab dolo 650 mg PO SOS
3.Tab. Levocetrizine 5mg PO SOS
4.Syrup ascoril 10 ml PO BD
5.tab. thyronorm 200mcg, PO OD
6.inj. optineruron 1 amp
7. BP temp charting 6th hourly
In view of common variable Immuno deficiency Immuno electrophoresis was sent which was normal.
UGI endoscopy was done showing no oesophageal varices.
He was referred to higher centre in view of portal hypertension secondary to ?NCPH/IPH, given the background of hypersplenism, massive splenomegaly with liver profile normal, portal vein doppler showing portal vein of diameter 1.6cms, with patent hepatic artery and vein, no collaterals and no ascites
He was also treated for tropical spleen with primaquine 30mg for 2 weeks, artemether and lumefantrine.
Bone marrow biopsy and lymph node biopsy showed reactive with no evidence of infiltrative etiology or malignancy in September.
20 days back he had history of pain abdomen and was admitted in the hospital in their vicinity and was advised splenectomy.
CT angiogram was done showing :
Brochoveolar lavage was advised I/v/o ground glass opacities and ? Halo sign to rule out fungal etiology.
Bronchoscopy video :
FNAC of cervical lymph node and thyroid was done showing metastasis
Bronchoalveolar lavage culture report showing -
KOH mount - no fungal elements seen
ZN staining showing - acid fast bacilli seen ( bronchoscopy contamination )
Direct smear - few inflammatory cells , few gram negative bacilli and few gram positive cocci in singles ( micrococci )
Culture - pseudomonas species grown ( contaminant )
Patient was taken for splenectomy on December 1st 2022
Liver biopsy report which was sent outside our hospital :
Spleen, Liver and mesenteric lymph node biopsy in our hospital :
Trends of hemogram post surgery :


























Comments
Post a Comment