Case 29 - A 70 year old male with altered sensorium
A 70 year old male came to casualty in the state of altered sensorium since one day cough with sputum ,SOB, burning sensation of oral cavity since 20 days
HOPI:
Patient was apparently asymptomatic 20 years back then had increased intake of alcohol
Cough associated with sputum small quantity, non foul smelling, non blood tinged.
Shortness of breath Initially class 2 gradually progress to class 4 since 30 days
With above complains patient was taken to government hospital treated symptomatically, patient was referred as his sensorium is detoriating
On presentation to casualty patient was drowsy but arousable tachypnic, afebrile, with oral cavity showing multiple erythematous vesicles over palate+
Past history:
Not a k/c/o HTN,ASTHMA,DM, EPILEPSY,CAD,CVA.
Personal history:
Diet: mixed
Appetite: decreased since 20 days
Bowel movements : normal
Bladder movements: decreased
No known allergies
H/O ALCOHOL CONSUMPTION PAST 30 YEARS 150ML/ALTERNATIVE DAY
LAST INTAKE 20 DAYS BACK .
Family history: not relevant
General examination:
Pt is drowsy, arousable,not cooperative
Pallor
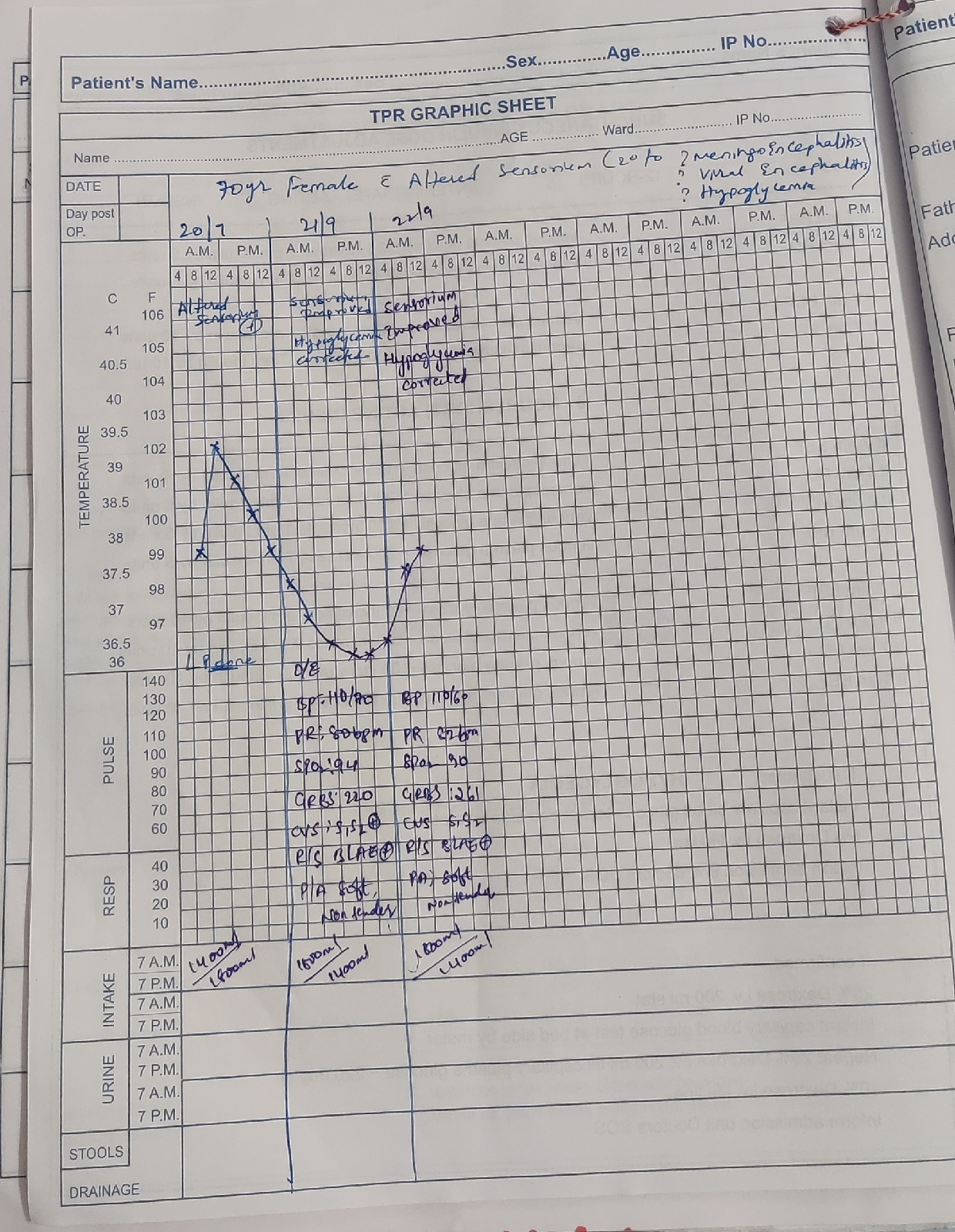
VITALS:
PR:133 BPM
RR:30CPM
BP: 120/90 MM HG
SPO2: 96% @ 15 litres of oxygen
systemic examination:
CVS: S1,S2+
RS : BAE+
P/A : SOFT,NT
CNS: ALTERED SENSORIUM
INVESTIGATIONS:
CBP,CUE,ABG,RFT,XRAY,PT,APPT,INR
ASSESSMENT:
ALTERED SENSORIUM SECONDARY TO UREMIC ENCEPHALOPATHY
VIRAL PNEUMONIA
AKI SECONDARY TO SEPSIS
PLAN OF CARE:
1) IVF (NS,RL,DNS) - Urine output+30 ml/h
2) 2)Head end elevation
3) 3) Oxygen inhalation to maintain SpO2 > 94%
4) 4) Inj. Augmentin 1-2 gm IV/BD
5) 5) Inj. Lasix 40 mg IV/BD
6) 6) Tab. Azithromycin 500 mg RT/OD
7) 7) Nebulisation with budecort 12th hrly, ipravent 4th hrly, mucomist 2nd hrly followed by chest physiotherapy
8) 8) Syp. Ambroxyl 15 ml RT/TID
9) 9) Mucopain gel L/A BD
10) 10) Betadine mouth gargles TID
11) 11) I/O and temperature charting
12) 12)GRBS 6th hrly











Comments
Post a Comment