CASE 8 - A 48 YEARS OLD FEMALE WITH DKA AND CVA
This is an E logbook to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here, we discuss our individual patient's problems through series of inputs from an available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence-based inputs. This E-logbook also reflects my patient-centered online portfolio and your valuable inputs in the comments are welcome.
I would like to thank Dr. Sai Charan sir ( General Medicine PG) for providing all the information related to the case.
CASE DISCUSSION :
This is the case of a 48 years old female who came to the hospital on 10th May, 2021 with :
CHIEF COMPLAINTS :
1) LEFT SIDED WEAKNESS (BOTH UL & LL) SINCE 3 DAYS
2) ALTERED SENSORIUM SINCE 10th MORNING
3) ABDOMINAL DISTENSION SINCE 10th MORNING
HISTORY OF PRESENT ILLNESS :
Patient was apparently asymptomatic 3 days back then she developed left sided weakness which was gradual and associated with tingling sensation so she was admitted in the outside hospital and there the treating doctor found acute infarcts on CT scans and I/V/O uncontrolled sugars patient was referred to the present hospital for further evaluation.
HISTORY OF PAST ILLNESS :
No H/O similar complaints in the past
K/C/O DM Type-2 since 2 years
K/C/O HTN since 3 days (No anti-hypertensive medication was taken)
PERSONAL HISTORY :
Appetite : Normal
Diet: Mixed
Bowel habits : Regular
Micturition : Abnormal
No known allergies
No addictions
FAMILY HISTORY : Insignificant
GENERAL EXAMINATION :
Patient was examined in a well-lit room after obtaining a valid consent
Pallor: Absent
Icterus: Absent
Cyanosis: Absent
Clubbing: Absent
Lymphadenopathy: Absent
Oedema: Absent
VITALS:
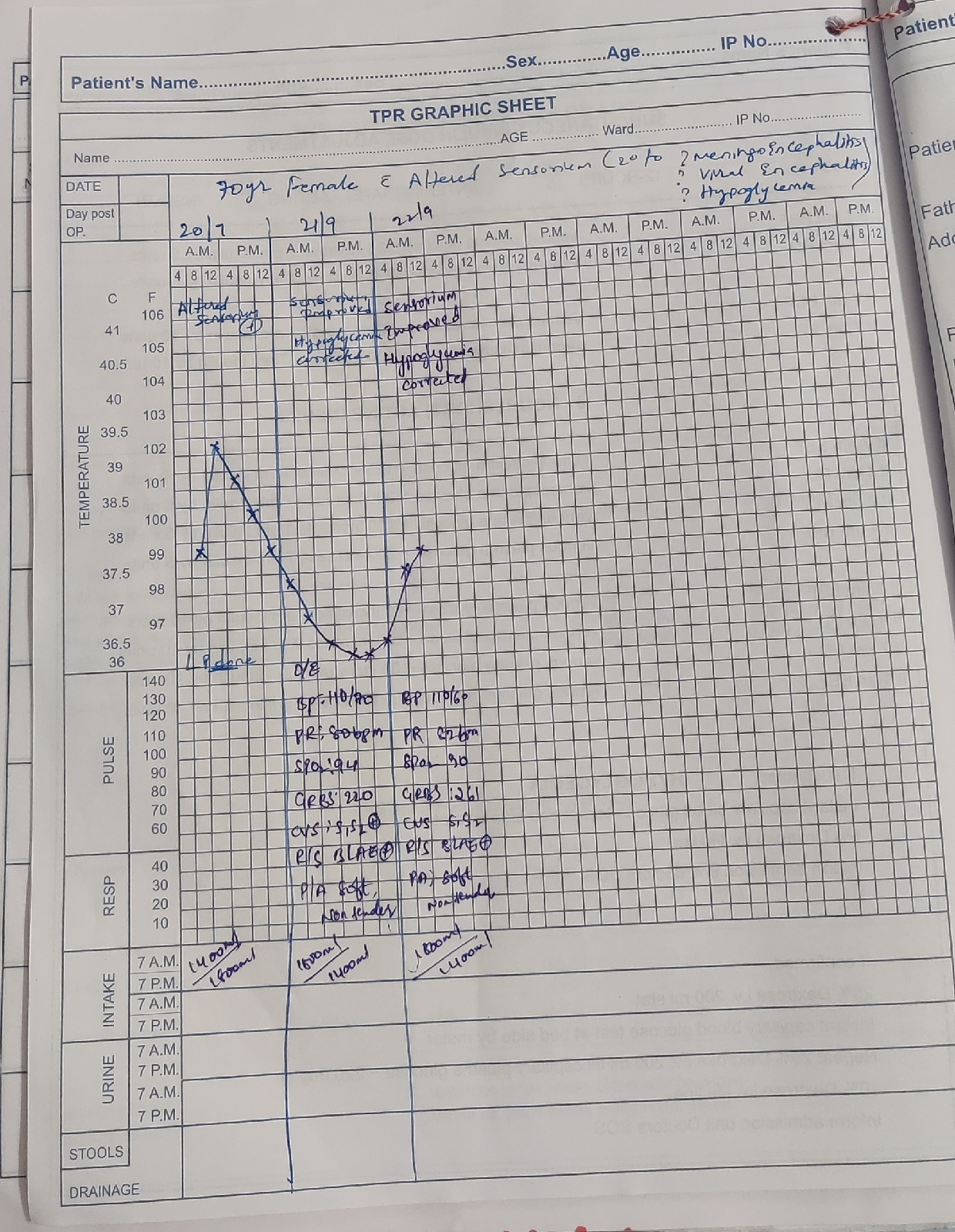
10th May
Temperature: Afebrile
Pulse Rate: 127 bpm
Respiratory Rate: 40 cpm
Blood Pressure: 150/90 mmHg
SPO2 : 92% at RA
GRBS: 453 mg%
11th May, 8:00am
BP: 110/80 mmHg
PR: 92bpm
TEMP: 92 F
GRBS: 141 mg/dl
11th May, 7:00pm
Temp: Febrile to touch
PR: 142 bpm
BP: 160/110 mmHg (T.MET-XL 25mg given)
12th May, 8:00am
BP: 130/80 mmHg
PR: 108 bpm
RR: 30cpm
GRBS: 111 mg/dl
12th May, 7:00pm
Temp: Afebrile to touch
BP: 120/70mm Hg
PR: 123 bpm
13th May, 8:00am
Temp: 2 fever spikes, 104 F
BP: 90/60mmHg
PR: 140 bpm
SYSTEMIC EXAMINATION :
CARDIO VASCULAR SYSTEM:
- S1 and S2 heard
- No thrills , no murmurs
RESPIRATORY SYSTEM:
- Bilateral air entry present and vesicular breath sound heard
- Dyspnea present
- Trachea is central in position
- NVBS +
- B/L Infrascapular crepts +
PER ABDOMEN:
- Distended abdomen
- No tenderness
- Bowel sounds heard
CENTRAL NERVOUS SYSTEM:
- Patient is drowsy
- Speech: No response
- Unable to test signs of meningeal irritation, cranial nerves, motor system, sensory system, GCS
- Patient is drowsy
- HMF intact
- Patient is comatose
- Doll's Eye : positive
- Gag reflex: positive
- Plantar reflex: mute
- Patient is comatose
- Doll's Eye : negative
- Pupils: Fixed, dilated
- Gag reflex: positive
- Plantar reflex: mute
- Patient is comatose
- Doll's Eye : negative
- Pupils: Fixed, dilated
- Plantar reflex: mute
- Urea: 38
- Creatinine: 1.2
- Ca+2 : 9
- Na+ : 138
- K+ :3.3
- Cl : 103
- Urea: 70
- Creatinine: 1.1
- Na+: 149
- K+: 3.9
- Cl: 107
- Hb: 11.7
- TLC: 8,200
- Platelet count: 2.42L
- Normocytic normochromic blood picture
DIAGNOSIS :
TREATMENT:
10th May
- INJ. INSULIN 6IU/IV/STAT
↓
- INJ. INSULIN 1ml in 39ml NS (1ml →40IU) @ 6ml/hr (↑/↓ acc.to algorithm 1)
- NBM till further orders
- IV fluids 1 ๏ NS ,1 ๏ RL } 1st 5 hr: 3.5-5L
- FOLEY'S CATHETER
- STRICT I/O MONITORING
- ANTI-PLATELETS AND MANNITOL AFTER INFORMING FACULTY
- INJ. MANNITOL 100ml/IV/TID
- T.ECOSPIRIN AV (75/10) mg PO/OD
- T.CLOPIDOGREL 75mg PO/OD
- INJ. INSULIN (HAI) 1ml in 39ml NS @ 3ml/hr (↑/↓ acc.to algorithm 1)
- NBM till further orders
- IVF- NS, RL @ UO+50ml/hr
- BP/PR/TEMP MONITORING 2nd HOURLY
- GRBS CHARTING HOURLY
- STRICT I/O CHARTING
- INJ. MANNITOL 100ml /IV/TID
- TAB. ECOSPIRIN 75mg PO/OD
- TAB. CLOPITAB 75mg PO/OD
- TAB. ATORVAS 40mg PO/HS
- HOURLY GRBS
- INJ. HAI (40-40) @8ml/hr
- TEPID SPONGING
- HEAD END ELEVATION 45०
- AIR/WATER BED
- ORAL SUCTION 2nd HOURLY
- T. MET-XL 25mg/RT/OD
- BP/PR/TEMP HOURLY
- Consider IVF O.45/NS, 5/Dextrose } @ 100ml/hr till NBM is stopped
- CST as per unit
- T. PCM 500mg/RT/SOS
- T. IVABRADINE, 5mg/RT/Stat.
- INJ.DEXMEDITOMIDINE 2amp in 46ml NS - 10ml/hr
- INJ.39 ml NS with 40IU HAI @6ml/hr
- INJ.AUGMENTIN 1.2gm/IV/BD
- INJ.CLEXANE 40mg/SC/BD
- Propped up position with change in position 2nd hourly
- INJ. HAI 40 IU in 39ml NS @ 4ml/hr ↑/↓ acc.to algorithm 1
- IVF- NS, RL @ UO+50ml/hr
- INJ. MANNITOL 100ml /IV/TID
- TAB. ECOSPIRIN 75mg PO/OD
- TAB. CLOPITAB 75mg PO/OD
- TAB. ATORVAS 40mg PO/HS
- INJ. DEXMEDETOMIDINE (2amp= 200μcg) in 48ml NS @ 5ml/hr (20μg/hr) ↑5ml/hr
- BP/PR/TEMP MONITORING 4th HOURLY
- GRBS CHARTING 6th HOURLY
- STRICT I/O CHARTING
- AIR/WATER BED
- PROPPED UP POSITION UPTO 45०
- IVF O.45/NS (in case of hypernatremia) 5/Dextrose-SOS
- INJ. PANTOP 40mg/IV/OD
- INJ. AUGMENTIN 1.2gm/IV/BD
- MANNITOL
- INJ.CLEXANE 40mg S/C -BD as per unit instructions
- GRBS 4th HOURLY
- RT FEEDS 50ml WATER HOURLY, 100ml MILK 4th HOURLY ,PROTEIN POWDER TID
- INJ.DEXMEDITOMIDINE 2amp(200mcg) in 46ml NS @ 5ml/hr
- TARGET PCO2 25-35mmHg
- INJ.HAI S/C 6th HOURLY MAINTAIN GRBS 100-250 mg/dl
- INJ.1 amp KCL IN IONS ( started at 4:oopm upto 10:00pm)
- TEMP/BP/PR HOURLY
- T.MET-XL 50mg/RT/OD
- AIR/WATER BED
- PROPPED UP POSITION
- IVF- NS: 0.9% @ UO+50ml/hr , 5 D- SOS
- INJ.NEOMOL 1gm/IV/SOS (if temp>101 F)
- INJ.PANTOP 40mg IV/OD
- INJ.AUGMENTIN 1.2gm/IV/BD
- INJ.CLEXANE 40mg S/C BD
- INJ.DEXMEDITOMIDINE 2amp(200ml) in 46ml NS @ 5ml/hr
- INJ.HAI S/C 6th HOURLY
- TAB.MET-XL 25mg RT/OD (if SBP> 140 mmHg)
- BP/PR/SPO2 MONITORING
- TEMP MONITORING 4th HOURLY
- STRICT I/O CHARTING
- INJ.ZOSTOM 1.5gm/IV/TID
- INJ.MANNITOL 100ml/IV/TID
- INJ.METROGYL 100ml/IV/BD
- INJ.ARTESUNATE 120mg/IV/0,12,24,48
- BP and PR : NON RECORDABLE
- CPR INITIATED
- INJ.ADRENALINE 1CC
- INJ.ATROPINE 1 CC GIVEN







Comments
Post a Comment