thanks Dr. NIKHILASAMPATH (Intern)
https://nikhilasampathkumar.blogspot.com/2021/05/a-48-year-old-male-with-seizures-and.html?m=1
A 48-year-old gentleman hailing from a small town in Telangana presented to the casualty ward on 25th April 2021 at 7:40am with the chief complaints of unresponsiveness for 7 hours and 3 intermittent episodes of seizures in the past 3 hours
HISTORY OF PRESENTING ILLNESS
The patient was apparently asymptomatic 7 hours ago(at 1am) when he suddenly became drowsy and stopped responding to verbal instructions.
Nearly 3 hours later (at 4am) he developed involuntary jerky movements on all four limbs, without regaining consciousness in between. He had 3 such episodes in total in a span of 3 hours. The duration of each episode is not known as the attendant failed to recollect the exact events
He has a history of binge drinking 3 hours prior to the onset of drowsiness ie. at 10pm on 24th April 2021.
A CT scan of the brain and an ECG were ordered as a part of the investigation. The CT scan showed an acute cerebral hemorrhage of the frontal, parietal and temporal lobes with a 13mm midline shift. It was decided that the patient requires neurosurgical intervention and he was referred to a higher center after informing his attendants. The patient was discharged from hospital#1 at 10:30am on 25th April 2021.
The patient reportedly lost complete consciousness on the way to the referred hospital#2. On arrival at hospital#2, he was redirected to another hospital due to a shortage of beds.
At hospital#3, it was apparently declared that the patient had become comatose. He was intubated for mechanical ventilation. Medical management given at hospital#3 is not known.
He stayed at hospital#3 till he reportedly died from a second case of intracranial bleeding on 25th April 2021.
PAST HISTORY
History of multiple falls when inebriated and history of minor head injuries that were left unattended. History of change in gait since 1 year
No history of fever, neck rigidity, or persistent headache
No history of Covid
Not a known case of Hypertension, Diabetes, Asthma, or Epilepsy.
PERSONAL HISTORY
Diet: Mixed
Appetite: Normal
Sleep: Normal
Bowel, bladder: Regular
Addicted to alcohol for the past 3 years. According to the attendant he used to drink "a few bottles per day". Drinks both bottled liquor and toddy.
DRUG HISTORY
No known drug allergies.
FAMILY HISTORY
No similar complaints in the family
No history of epilepsy, diabetes, hypertension, asthma, or TB in the family
GENERAL EXAMINATION
At the time of admission, on examination in a well-lit room and with the informed consent of the patient's attendant
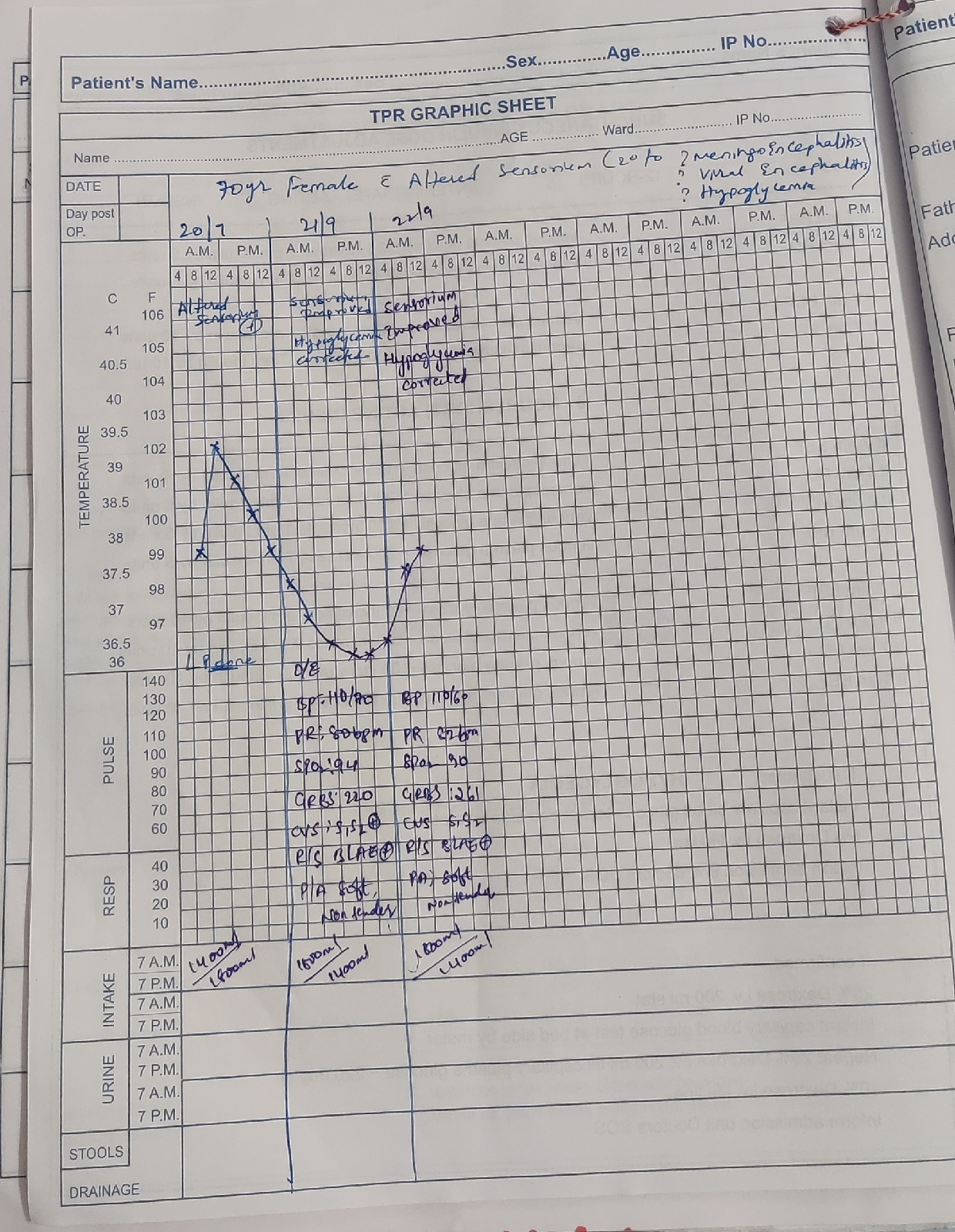
- The patient is conscious with altered sensorium
- He was moderately built and well-nourished
Pallor: Absent
Icterus: Absent
Cyanosis: Absent
Clubbing: Absent
Lymphadenopathy: Absent
Edema: Absent
Vitals: On admission,
Temperature: Afebrile
PR: 102bpm
BP: 150/90mmHg
SpO2: 62% at RA
GRBS: 156mg%
SYSTEMIC EXAMINATION
Respiratory System: Bilateral air entry positive
CVS: s1, s2 heard
CNS: Altered sensorium noted, E1V1M1
P/A- Soft, non-tender
INVESTIGATIONS
1) ECG (25/04/21)
2) CT Brain (taken on 25/04/21)
PROVISIONAL DIAGNOSIS
Generalized tonic-clonic seizures secondary to acute hemorrhage in the frontal, temporal, and parietal lobes with a 13mm midline shift
TREATMENT ADMINISTERED
Ryles Catheterization
Head end elevation, Oxygenation
INJ Lorazepam stat 2CE
INJ Levetiracetam 1gm IV stat
INJ Mannitol 100ml IV stat
INJ Thiamine 1 ampoule in 100ml normal saline IV stat





Comments
Post a Comment