Case 30 - 55 yrs old male patient with cheif complaints of an episode of generalised jerky movements of upper and lower limbs 4 hours ago
A 55 year old man was rushed to the emergency room by his family with complaints of generalised jerky movements of upper and lower limbs, lasting for 2 minutes, that occurred 4 hours ago at 4 AM in the night.
Patient was apparently asymptomatic until yesterday night, when he had sudden jerky movements of upper and lower limbs, associated with loss of consciousness and involuntary micturition back. The patient is disoriented to time, place but recognises his family, there is post ictal confusion. The patient feels tired and week. There are no signs of tongue bite or fracture of long bones. Upon further inquiry the patient gives history of consumption of alcohol (650ml) for 2 days (3 days prior to presentation) continuously, subsequently, 2 days back he developed abdominal pain which is dragging type, localised to the right upper quadrant and associated with altered sensorium.
Review of systems revealed :-
C/o chest pain, dragging type, non radiating to left arm.
C/o vomiting 3 days back, non bilious, not projectile, with food particles as contents
Past history:-
Patient is k/c/o DM since 2 yrs and on oral hypoglycemic drugs.(Glimi M2)
Patient never had history of similar episodes in the past.
He has no history of any CAD or CVA.
Personal history:-
Alcohol consumption since 30 yrs and currently consumes 650 ml of alcohol daily.
The person has a 30 pack year smoking history. (10 beedis/day)
On examination patient is conscious, irritable
Vitals:-
BP- 120/70 mmHg
PR-111 bpm
Spo2- 99%at RA.
GRBS-
5:30-600
7:30- 390
8:30-380
9:30- 383
10:30- 382
11:30- 260
12:30- 210
1:30- 220
2:30- 206
3:30- 207
4:30- 147
5:30- 77
6:30- 121
7:30- 131
Clinical exam pictures :-
CVS - S1, S2 heard, no murmurs, no JVP observed, neck veins not distended
RS - respiratory rate - 22 cpm, no adventitious breath sounds heard
CNS - patient is in altered sensorium, irritable and irrelevant talk; GCS - 11/15
P/A - abdomen is soft , non distended, scaphoid in shape, patient complains of pain in RUQ, liver appears to be enlarged, spleen not palpable.
Lab investigations :-
Treatment:-
1. IVF- NS- 1L for 3hrs.
2. Inj HAI 6IU IV/STAT.
3. GRBS monitoring hrly.
4.IVF-5% Dextrose if GRBS<250mg/dl.
5.Inj THIAMINE 100mg in 100 ml NS/IV/BD.
6.Inj OPTINEURON 1 amp in 100ml NS/IV/OD.
PROVISIONAL DIAGNOSIS:-
Diabetic ketoacidosis with known case of diabetes mellitus.
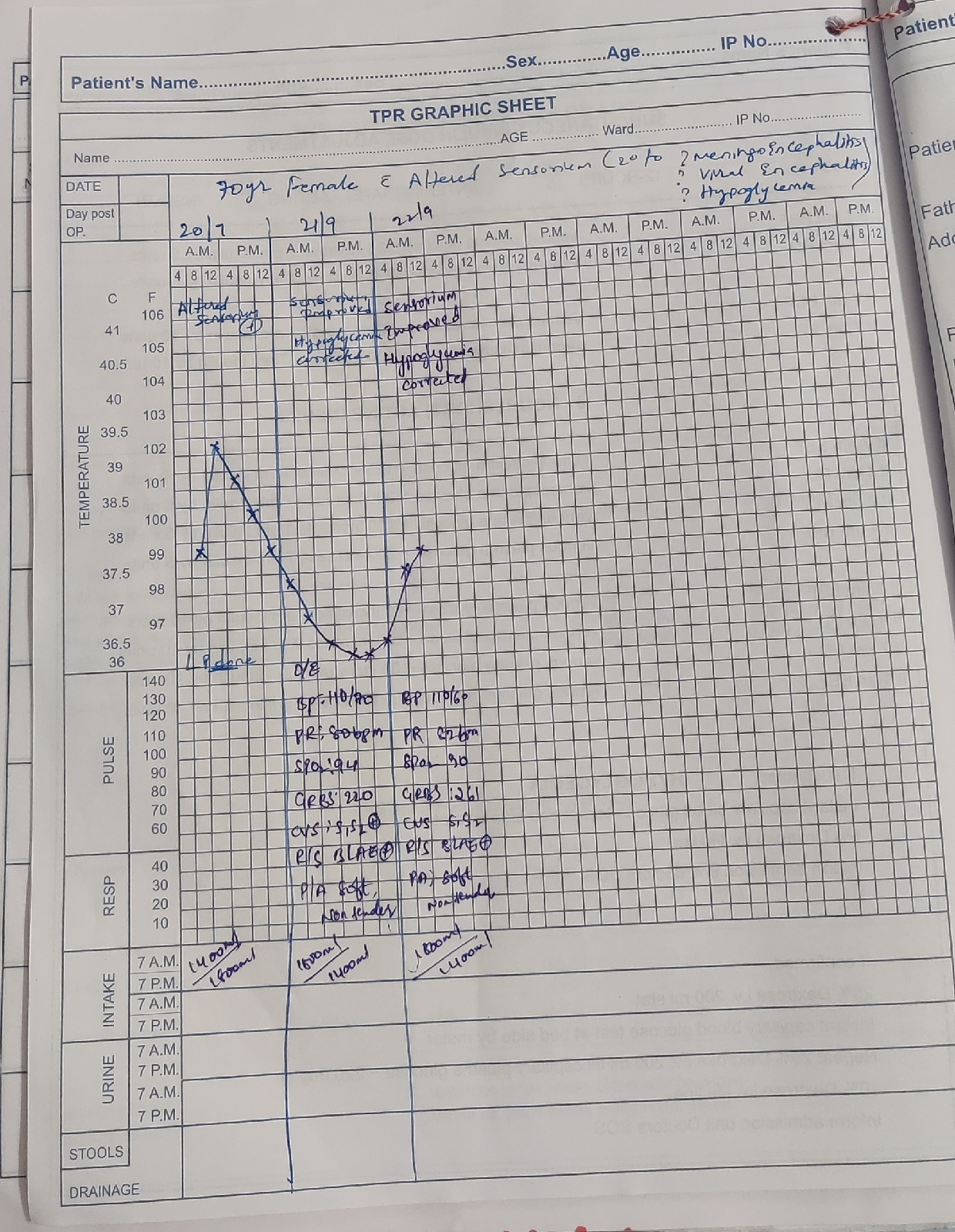
Day 1
S
Sensorium improved
Abdominal pain - mild tenderness in RUQ, subjectively less than yesterday
No new episodes of seizures, vomiting, diarrhoea
No new complaints
O
Patient is conscious, coherent, cooperative
Temp- 98.4 F
BP- 110/60 mmHg
PR- 95 bpm
RR- 20 cpm
SPO2- 98% on RA
GRBS- 130 mg/dL
CVS- S1, S2 +
RS - BAE +; Trachea- Central
P/A- Soft, non distended, mild tenderness in RUQ, BS +
CNS- sensorium improved, oriented to time place and person, GCS - 13/15
A
Diabetic ketoacidosis with known case of diabetes mellitus.
P
1. IVF- NS- 1L for 3hrs.
2. Inj HAI 6IU IV/STAT.
3. GRBS monitoring hrly.
4.IVF-5% Dextrose if GRBS<250mg/dl.
5.Inj THIAMINE 100mg in 100 ml NS/IV/BD.
6.Inj OPTINEURON 1 amp in 100ml NS/IV/OD.
Day 2
S
Sensorium improved
no complaints of abdominal pain
No new episodes of seizures, vomiting, diarrhoea
No new complaints
O
Patient is conscious, coherent, cooperative
Temp- 97.4 F
BP- 120/60 mmHg
PR- 88 bpm
RR- 18 cpm
SPO2- 99% on RA
GRBS- 124 mg/dL
CVS- S1, S2 +
RS - BAE +; Trachea- Central
P/A- Soft, non distended, BS +
CNS- sensorium improved, oriented to time place and person, GCS - 15/15
A
Diabetic ketoacidosis with known case of diabetes mellitus.
P
1. IVF- NS- 1L for 3hrs.
2. Inj HAI 6IU IV/STAT.
3. GRBS monitoring hrly.
4.IVF-5% Dextrose if GRBS<250mg/dl.
5.Inj THIAMINE 100mg in 100 ml NS/IV/BD.
6.Inj OPTINEURON 1 amp in 100ml NS/IV/OD.












Comments
Post a Comment