This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 65 year old female patient brought to casuality with
Cc: involuntary movements of B/L upper and lower limbs from 5pm (i.e5/10/22). And altered sensorium(post ictal confusion) from 5pm
History of present illness:
Patient was apparently a symptomatic one year back then she developed right upper limb and right lower limb weakness diagnosed to have right hemiparesis.From 1st october patient developed seizures for which she went to Bhongiri Area hospitaland was given phenetoyin 100mg tid, levipril 500mg BD but while shifting the patient she had 5 to 6 episodes of seizures .Since yesterday evening 5:00 pm she developed continous involuntary movements each lasting for 2-3 mins and post ictal confusion for 2-3 minutes.H/O Up rolling of eyeball the present tongue bite present,H/O involuntarymicturition present,H/O involuntary passage of stools present.
Past history:
Old CVA one and half year back ,Right sided hemiparesis (now able to walk with stick)
DM and HTN since 1 and half year back
No H/o asthma,TB
Personal history:
DIET: MIXED
APPETITE: Decreased since 1 week
BOWEL AND BLADDER: REGULAR
NO ALLERGIES
Addiction: toddy drinker daily for 30years (quater) and stopped1and 1/2 year back
Family history:
No relevant family history
General examination:
Pateint is not C/C/C and not oriented to time ,place and person
PALLOR +
NO CYANOSIS
NO CLUBBING
NO ICTERUS
NO LYMPHADENOPATHY
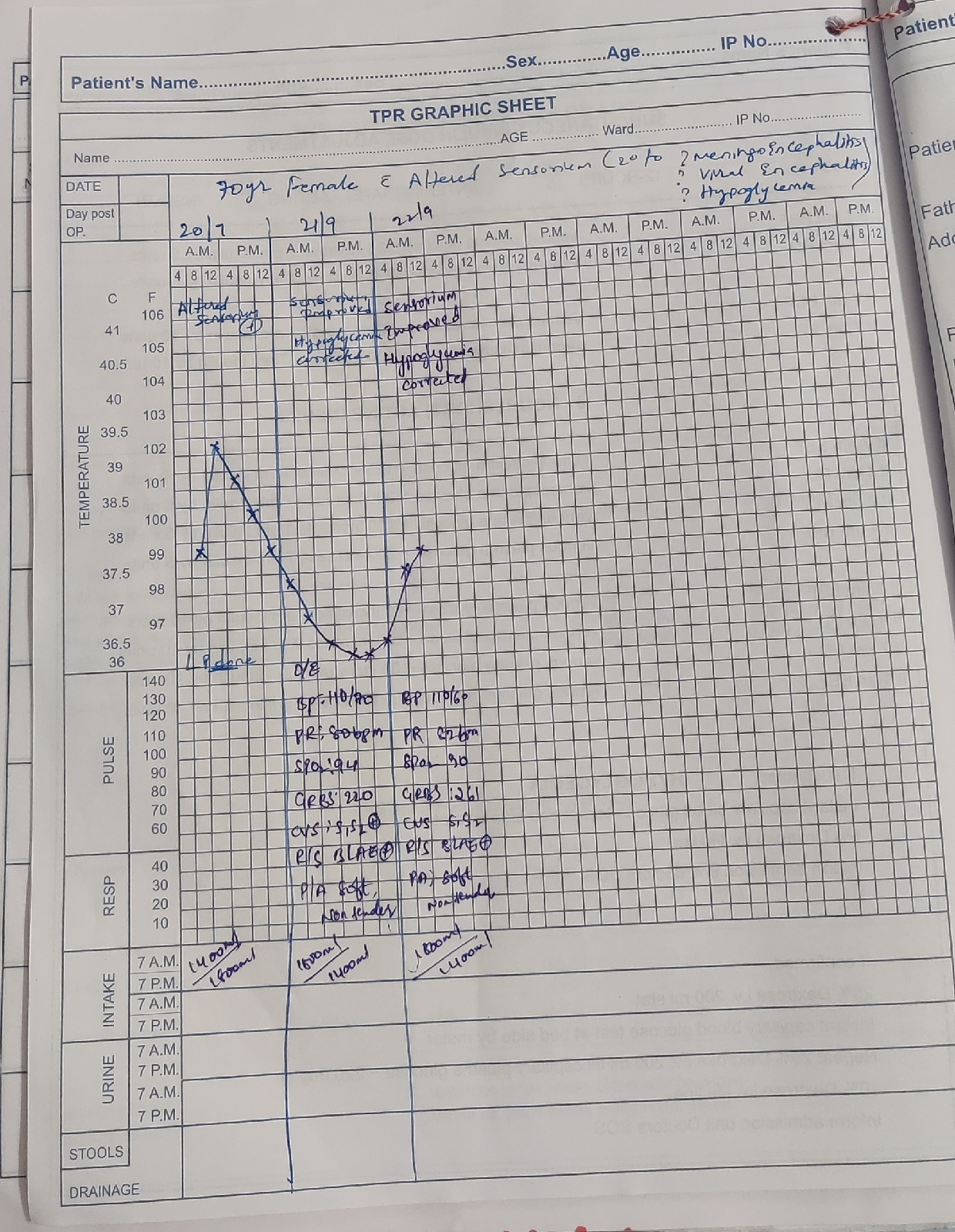
VITALS:
Temp-97.3°F
BP-100/60 MMHG
PR-54 BPM
RR-12 CPM
SPO2 - 98% @RA.
GRBS: 334mg/dl
Systemic examination:
CVS:
S1,S2 heard
No thrills,murmurs
RS:
BAE+, B/L CREPTS-
P\A:
SOFT, DIFFUSE TENDERNESS ,GUARDING PRESENT
CNS:
HMF
not oriented to time, place and person
Pupils: B/L pin point non reacting to light
FOM: +
Speech: slurred
Cranial nerve examination: could not be elicited
no deviation of angle of mouth
Motor Examination:
Power R L
UL 2/5 3/5
LL 0/5 3/5
Tone R L
decreased decreased
decreased decreased
Reflexes: B T S K A P
R 3+ 3+ 3+ 3+ 2+ mute
L 2+ - - 2+ 1+ mute
Cerebellar signs : could not be elicited
Investigations:











USG ABDOMEN:
Liver : N S/increased E
PV AND CBD: normal
Gall Bladder : distended
Pancreas: N S/E I/O 36X35mm cyst in upper pole of kidney
RT. Kidney: 8.6x 3.4 cm N S/e
LT. Kidney : 8.7x3.5 cm
Aorta IVC: N
No Ascites
No Lymphadenopathy
Urinary bladder: partially distended
IMPRESSION:
1. Left renal cortical cyst
2. Grade 2 fatty liver
MRI BRAIN OBSERVATION :Old lacunar infact in left corona radiator .Rest of the cerebral
parenchyma shows normal grey/white matter differentiation ,basal ganglia and thalami are normal,brainstem and cerebellum normal ,craniovertebral and cervicomedullary Junction are normal .sella,pituitary and parasellar region are normal .stalk and hypothalamus are normal .posterior pituitary bright spot is normal ,no evidence of abnormal calcification , haemorrhage or vascular abnormality on SWI sequence ,orbit and globe content are normal.
IMPRESSION: Old lacunar infact in left coronaradiata
PROVISIONAL DIAGNOSIS:
STATUS EPILEPTICUS 2 TO RECCURENT CVA (LEFT CAPSULOGANGLIONIC) DUE TO ?
CARDIOEMBOLI WITH OLD AWMI ,HTN AND DM AND COMPLETE HEART BLOCK
Treatment Given:
1 . IV fluids NS with optineuron RL 75ml/hr
2.RT feeds 50ml water 2hrly 100ml milk with protein powder4hrly
3.inj levetiracetam 1gm/iv/bd
4.Tab .eptioin 100mg RT/TID
5. Inj human actrapid insulin s/c TID
6.syp potklor 20ml/RT/BD
7.GRBS charting
8.Lorazepam inj. 2cc iv /sos
9.w/f seizure activity
10. BP,PR,spo2,RR temp charting













Comments
Post a Comment